Neuromonitoring is a technique that enables the real-time monitoring of neural system functions, particularly during neurosurgical procedures. In the field of neurosurgery, the preservation of neural pathways and brain functions is of critical importance. With neuro-monitoring methods, neural stimuli can be detected instantaneously, allowing surgical strategies to be adjusted in real-time. This technological approach helps ensure that surgery is performed safely and effectively.
The Role of Neuromonitoring in Neurosurgery
Neuromonitoring plays a crucial role in protecting neural pathways during intraoperative neuromonitoring, especially in high-risk brain and spinal surgeries. Techniques such as EMG, EEG, SEP, MEP, BAEP, and VEP enable the real-time monitoring of neural function during brain surgeries. These neuromonitoring technologies allow surgeons to detect changes in neural activity during surgery and make necessary adjustments to their approach.
Given the delicate and high-risk nature of brain surgery, the importance of neuromonitoring becomes even more evident. Neurosurgeons, neurologists, and neuromonitoring technologists work closely together to ensure that the process runs smoothly and safely. While neurologists interpret data to assess the healthy functioning of neural pathways, neuromonitoring technicians ensure the proper functioning of the equipment, collect signals, and provide real-time information to the surgeon. This collaboration is essential in safeguarding neural integrity and minimizing complications.
Neuromonitoring Techniques
Neuromonitoring can be performed using a variety of techniques, which may vary depending on the type of surgery and the patient’s condition. The most commonly used neuromonitoring techniques include:
- Intraoperative Motor Evoked Potential (MEP) Monitoring: Motor evoked potentials (MEP) measure the electrical responses to stimuli that cause muscle contractions. This method is commonly used in brain and spinal surgeries to monitor the safety of nerve roots and the spinal cord. MEP enables rapid detection of any changes in nerve activity.
- Somatosensory Evoked Potentials (SSEP): Sensory evoked potentials (SSEP) measure the electrical responses from the sensory nervous system to electrical stimuli applied to the body. This technique continuously monitors nerve conduction during brain and spinal surgeries. Abnormal SSEP responses alert the surgeon to reevaluate and adjust the surgical procedure as needed.
- Electroencephalography (EEG): EEG measures the electrical activity of the brain and is particularly useful in monitoring brain function during surgery. This technique is crucial in detecting abnormal brain activity, such as seizures or ischemic changes, that could indicate neural compromise. EEG is commonly used in brain surgeries to ensure that critical brain regions are not damaged during the procedure. It also helps in monitoring the depth of anesthesia, ensuring that the patient’s brain activity is properly managed during surgery.
- Electromyography (EMG): Electromyography (EMG) records the electrical activity of muscles, particularly useful in monitoring peripheral nerves and nerve root activities. Surgeons can detect abnormal electrical activity in muscles using EMG, allowing for the early identification of potential neural damage.
- Brainstem Auditory Evoked Potentials (BAEP): BAEP (Brainstem Auditory Evoked Potentials) measures the electrical responses from the brainstem to auditory stimuli. This method monitors brainstem function. Particularly useful during brain and spinal surgeries, BAEP evaluates the communication between auditory pathways and the brainstem. Surgeons can detect functional changes in the brainstem and adjust the procedure to minimize damage to neural pathways.
- Visual Evoked Potentials (VEP): VEP is the measurement of the electrical responses generated by the brain to visual stimuli, such as a light or a specific visual pattern. This method is primarily used to assess the health and function of the visual pathways (optic nerves and visual cortex). VEP is typically used to detect conditions that may affect the visual system, which are not visible to the naked eye. This test is a crucial tool for monitoring and detecting damage in the visual pathways. The electrical responses recorded from the brain show how signals are transmitted from the eyes to the brain, allowing surgeons to monitor the preservation of the visual pathways in real-time.
- Brain Mapping: Brain mapping is a technique used to identify and locate critical functional areas of the brain before or during surgery. This can include identifying areas responsible for motor functions, sensory input, speech, and vision. Brain mapping, particularly through direct cortical stimulation, helps surgeons navigate around sensitive regions and avoid damaging essential brain structures. This technique is especially beneficial in brain tumor surgeries or when removing tissue in regions associated with critical functions.
- Awake Craniotomy: In an awake craniotomy, the patient is kept awake during the procedure, typically for surgeries involving the brain’s motor or speech areas. This technique allows surgeons to interact with the patient and assess their cognitive or motor responses in real time, helping to ensure that key functional areas are preserved. The use of neuromonitoring in awake craniotomy procedures, combined with direct feedback from the patient, enhances the surgeon’s ability to avoid or helps prevent damage to critical brain regions while performing necessary operations.
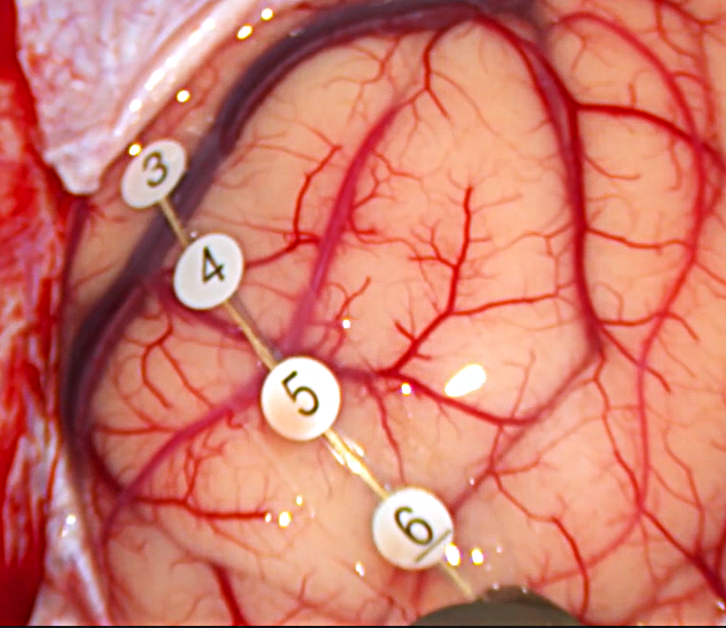
Brain Mapping © ENI
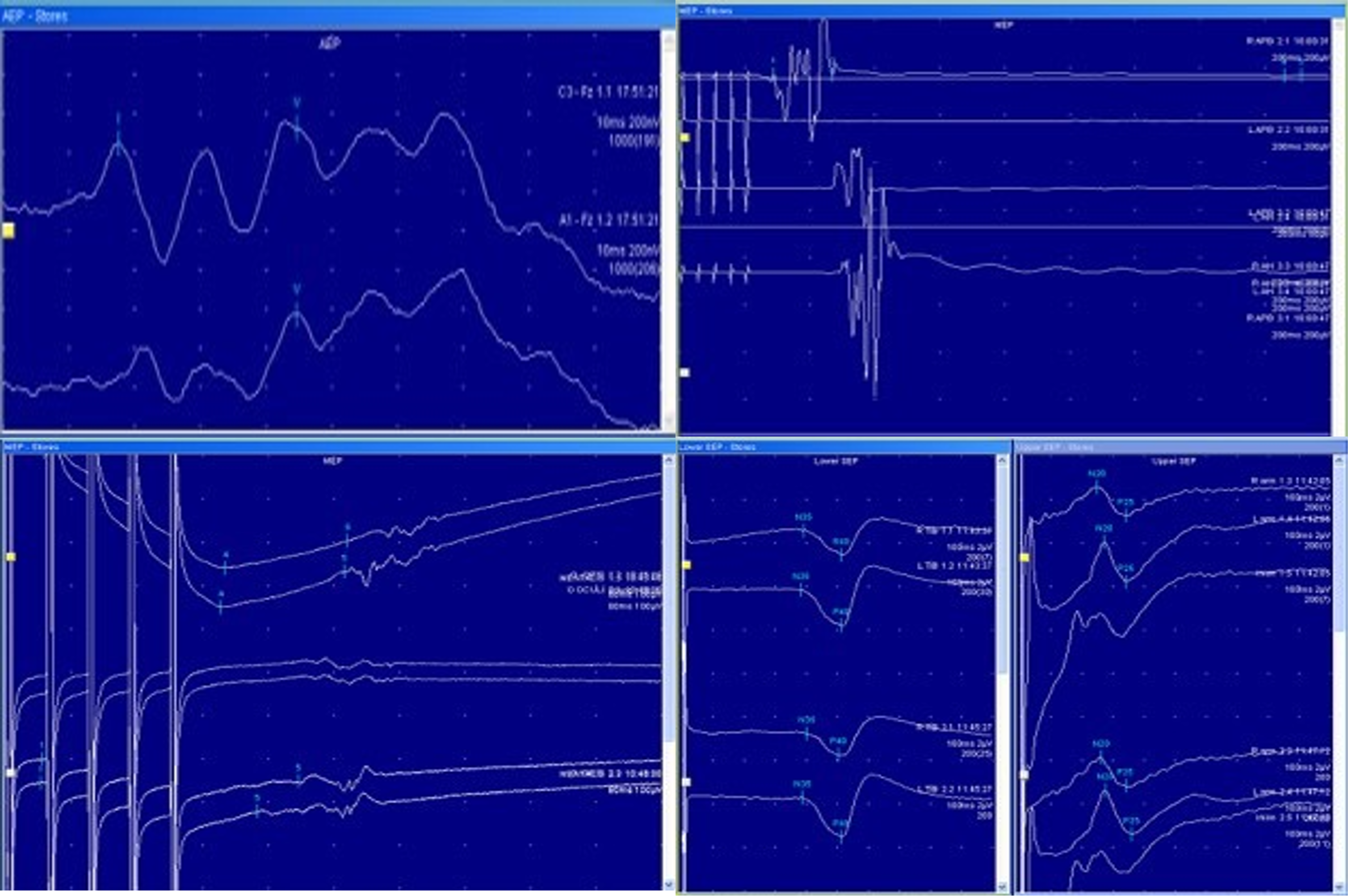
Neuromonitoring © ENI
How Neuromonitoring Works
Neuromonitoring is carried out by a specialized team before, during, and after the surgical procedure. The process generally involves the following steps:
- Preparation Phase: Before surgery, the patient’s clinical evaluation is conducted, and the necessary neuromonitoring methods are determined. Electrodes and electrode placement devices are carefully positioned on the patient’s body, targeting specific muscle groups, neural pathways, or the brain.
- Stimulation and Measurement Phase: According to the selected neuromonitoring technique, electrical stimuli are applied to the electrodes on the patient, and the neural responses are measured. Surgeons monitor these responses in real time.
- Data Analysis and Feedback: Data obtained by the neuromonitoring devices are analyzed by a computer system. If abnormal changes are detected, the system alerts the surgeon. Based on this feedback, the surgeon may adjust the surgical approach or intervene as needed.
- Interpretation of Results: Throughout the procedure, the surgeon continually reviews the neuromonitoring data. This provides a critical indicator of whether neural functions are at risk.
- Postoperative Monitoring: In some cases, postoperative monitoring of neural functions with neuromonitoring devices is necessary to detect potential issues during the recovery phase.
Advantages of Neuromonitoring in Neurosurgery
1.Minimization of Neural Damage:
• Real-Time Monitoring: Neuromonitoring enables the surgeon to observe neural pathways and functions in real time. Any abnormalities or risks of damage can be detected, allowing the surgeon to act promptly.
• Intervention in Critical Areas: In areas such as the brain, spinal cord, and peripheral nerves, neuromonitoring helps ensure the preservation of these critical structures. It helps prevent neural damage, contributing to better postoperative recovery for the patient.
2.Increased Surgical Safety:
• Early Detection of Risks: By monitoring neural conditions, neuromonitoring helps surgeons detect potential risks during surgery, enabling them to minimize complications through immediate interventions.
• Reduced Risk of Incorrect Interventions: Feedback from neuromonitoring devices aids the surgeon in making informed decisions, reducing the likelihood of damaging neural structures and enhancing surgical safety.
3.Improved Postoperative Recovery:
• Functional Feedback: Continued monitoring of the neural system after surgery helps the surgeon assess whether neural functions were adequately preserved during the procedure. Recovery is faster when neural functions are successfully preserved.
4.Faster and More Informed Decision-Making for Surgeons:
• Instant Feedback: Neuromonitoring data provide real-time information, assisting surgeons in making informed decisions during the procedure, ultimately improving the success rate of the operation.
• Management of Complicated Situations: In spinal surgeries, where neural pathways are at high risk, neuromonitoring helps ensure that any risks are detected, enabling immediate action to be taken.
5.Preservation of Neural Function:
• Monitoring Motor and Sensory Functions: Techniques such as MEP and SSEP continuously monitor motor and sensory pathways, helping preserve these functions throughout surgery.
• Safety in Tumor Resection: During brain tumor surgeries, where nearby neural pathways may be at risk, neuromonitoring technology helps ensure the safe removal of tumors without causing damage to critical neural structures.
6.Higher Success Rates in Brain and Spinal Surgery:
• Improved Success Rates: By minimizing the risk of neural damage, neuromonitoring directly contributes to higher success rates in neurosurgical procedures.
• Long-Term Benefits: Preserving neural functions leads to better long-term outcomes, enabling patients to enjoy a healthier life without functional loss.
7.Support for Multidisciplinary Collaboration:
• Collaboration Among Various Specialists: The neuromonitoring process involves collaboration among neurosurgeons, neurologists, monitoring technicians, anesthesiologists, and other healthcare professionals. This multidisciplinary approach ensures high-quality monitoring and assessment throughout the surgical process.
