What is a functional MRI?
Functional MRI (fMRI) is an advanced imaging technique that measures brain activity by detecting changes in blood flow associated with neural activity. When a specific brain region is activated, it requires more oxygenated blood, and fMRI captures these changes in blood oxygenation to map brain function in real time. Unlike conventional MRI, which provides structural images of the brain, functional MRI of the brain allows clinicians to visualize brain activity during cognitive, sensory, and motor tasks, providing crucial insights into how different brain regions contribute to various functions.
Applications
1.Mapping Critical Brain Areas for Surgical Planning:
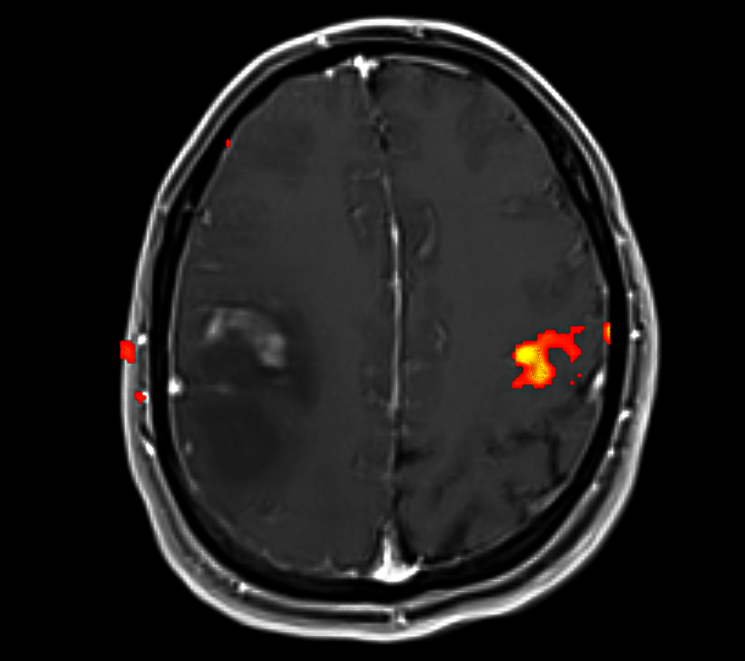
- Preoperative Brain Mapping: In patients requiring brain surgery, particularly for tumors, epilepsy, or vascular malformations, functional MRI of brain is essential for identifying and mapping critical functional areas of the brain, such as the motor cortex, sensory cortex, language centers, and visual centers. Knowing the exact location of these regions is crucial to ensuring that they are avoided or preserved during surgery to minimize the risk of neurological deficits after surgery.
- Functional Mapping for Tumor Resection: For patients with brain tumors, especially those located near or within functional regions, MRI functional helps identify the relationship between the tumor and critical brain functions. This allows neurosurgeons to plan the resection in a way that maximizes tumor removal while minimizing damage to essential brain areas. Tumors located near the motor cortex, speech areas, or visual pathways require careful planning to avoid impairing these vital functions.
Functional MRI © ENI
2.Surgical Planning for Epilepsy Treatment:
- Mapping Epileptogenic Zones: Brain functional MRI is increasingly used in epilepsy surgery to localize epileptogenic zones (regions of the brain where seizures originate). By identifying regions of abnormal brain activity or altered blood flow during seizure events, fMRI helps neurosurgeons plan procedures such as lobectomy or hemispherectomy while preserving key brain functions. This is particularly important for patients with drug-resistant epilepsy who may be candidates for surgical treatment to control seizures.
- Preoperative Planning for Hemispherectomy or Lesionectomy: For patients undergoing hemispherectomy (removal of one cerebral hemisphere) or lesionectomy (removal of an epileptogenic brain lesion), fMRI assists in determining the functionality of the brain tissue surrounding the epileptic focus, helping to preserve motor, sensory, and cognitive functions post-surgery.
3.Assessment of Brain Function in Motor and Sensory Disorders:
- Motor Function Mapping: For patients undergoing surgery for motor disorders, such as brain tumors near the motor cortex or surgeries involving spinal cord stimulation, functional MRI can help map the motor areas responsible for movement control. This ensures that the primary motor cortex, responsible for voluntary movement, is preserved during surgery, reducing the risk of postoperative motor deficits such as hemiparesis (partial paralysis).
- Sensory Function Mapping: Similarly, mri functional brain can map sensory areas of the brain, including regions involved in touch, pain, and temperature perception. This is crucial in surgeries where sensory function must be preserved, such as in the resection of brain lesions or tumors near sensory processing areas.
4.Language Mapping for Neurosurgical Planning:
- Broca’s and Wernicke’s Areas: fMRI plays a key role in language mapping, especially for tumors or lesions located in the dominant hemisphere (usually the left hemisphere) where Broca’s area (responsible for speech production) and Wernicke’s area (responsible for language comprehension) are located. By identifying the precise locations of these regions, fMRI helps guide neurosurgeons in planning tumor resections, ensuring that these critical areas are not damaged during surgery.
- Preoperative Language Function Assessment: In patients undergoing brain surgery for tumors or vascular malformations in the language-dominant hemisphere, fMRI helps assess language function and cognitive abilities prior to surgery. This enables surgeons to understand the patient’s baseline function and predict postoperative outcomes more accurately.
5.Monitoring Brain Function During Surgery:
- Intraoperative Brain Mapping: While intraoperative direct electrical stimulation remains the gold standard for mapping functional areas during surgery, fMRI can be used in preoperative planning and intraoperative monitoring to further refine the surgical approach. By visualizing the functional network of the brain, fMRI can assist in monitoring real-time activity during surgery, particularly in complex resections or functional surgeries (e.g., deep brain stimulation or stereotactic radiosurgery).
6.Assessment of Postoperative Recovery
- Post-Surgical Functional Changes: After neurosurgery, fMRI is used to evaluate neuroplasticity—the brain’s ability to reorganize and compensate for lost function. By assessing changes in blood flow and brain activity, fMRI can reveal how other brain regions may take over the functions previously controlled by the removed or damaged areas, helping guide postoperative rehabilitation and recovery strategies.
Advantages in Neurosurgery
1.Precise Localization of Functional Areas
- fMRI provides a non-invasive method for accurately mapping functional regions of the brain before surgery. This allows surgeons to avoid critical areas such as the motor cortex, sensory cortex, language areas, and visual centers, reducing the likelihood of postoperative deficits like motor weakness, sensory loss, or language impairments. The ability to map these areas with high precision is essential for minimizing risk during surgery and ensuring the best possible outcomes for patients.
2.Guiding Tumor Resection and Sparing Critical Function:
- In brain tumor resection, the ability to identify the relationship between a tumor and functional brain regions is vital for achieving maximal resection while minimizing damage to healthy tissue. fMRI allows surgeons to plan the tumor excision in a way that maximizes tumor removal while minimizing the risk of damaging functional brain areas, especially those responsible for language, movement, and cognition.
3.Preserving Cognitive and Motor Function:
- fMRI enhances surgical precision, helping neurosurgeons plan procedures to avoid damage to areas responsible for high-order cognitive functions such as language, memory, and executive functions. In patients with tumors or lesions near the precentral gyrus (motor cortex) or Broca’s and Wernicke’s areas (language centers), this technology significantly reduces the risk of neurological deficits such as aphasia, paralysis, or loss of sensation.
4.Aiding in Functional Neurosurgery:
- fMRI plays an important role in the planning of functional neurosurgical interventions such as deep brain stimulation (DBS) for Parkinson’s disease or stereotactic radiosurgery. By identifying and mapping the precise functional areas of the brain, surgeons can ensure that their interventions target the right regions while preserving adjacent, healthy tissue.
5.Enhancing Patient Selection for Epilepsy Surgery:
- In patients with drug-resistant epilepsy, fMRI helps identify epileptogenic zones and evaluate functional reorganization in the brain. This is particularly helpful in selecting appropriate candidates for surgical procedures like lobectomy or hemispherectomy, ensuring that the brain regions responsible for essential functions are preserved while treating the seizure focus.
